Varicocele
Non-surgical treatment for symptom relief and infertility
A varicocele is a network of dilated veins in the scrotum. In other words, it is the varicose veins of the scrotum. It feels like a “bag of worms” and can be unsightly to some. It may cause pain and discomfort, shrinkage of testis and infertility. The increased temperature in the scrotum and reflux of blood may shrink testis and decrease sperm production. It is the most common correctable cause of male infertility.

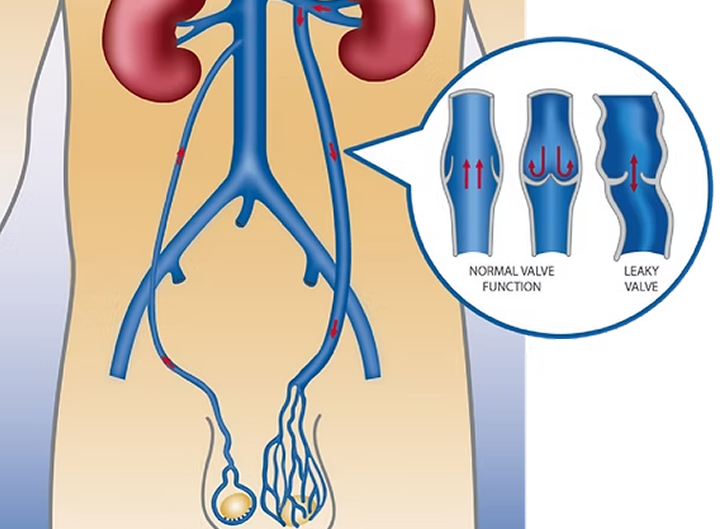
The testicular veins have a long course and drain the testes up to the level of the kidneys. Faulty valves in the testicular vein allow reflux (backflow) of blood down into the scrotum, causing congestion with pooling of stagnant blood and build up of pressure in the veins. The left side is far more common than the right.
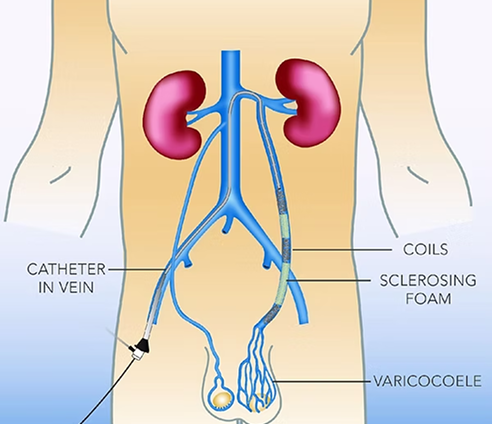
It is a non-surgical minimally invasive technique performed by an interventional radiologist in an angiography suite. Under light sedation and local anaesthetic, a small catheter (a tube less than 2mm) is inserted into the vein in the groin and directed under X-ray into the testicular vein. Reflux in the vein is then confirmed with X-ray dye and the refluxing testicular vein is blocked internally with coils and Fibroven foam.
Traditionally it is treated with surgical ligation. For more than 25 years, testicular vein embolisation has been used as an alternative.
It is performed in an operating theatre. The surgeon makes a skin cut above the scrotum, then dissects through the layer of tissues to expose the faulty veins, which are tied off, redirecting venous return via other healthy pathways.
It is a non-surgical minimally invasive technique performed by an interventional radiologist in an angiography suite. Under light sedation and local anaesthetic, a small catheter (a tube less than 2mm) is inserted into the vein in the groin and directed under X-ray into the testicular vein. Reflux in the vein is then confirmed with X-ray dye and the refluxing testicular vein is blocked internally with coils and Fibroven foam.
Treatment is recommended if there are symptoms such as pain and discomfort, if the testis is smaller or the sperm count is low.
The success rate is above 90% for both surgery and embolisation. Improved sperm count and motility were shown in 75% of patients. Subsequent pregnancy rate varies between 30-60% after treatment.
The recurrence rate is around 10% for surgery and less with modern embolisation technique using coils and Fibrovein. Surgical failure can be treated by embolisation and vice versa. Embolisation failure can be treated by repeating embolisation.
Surgical method requires micro dissection of the groin region. There are the risks of injury to the vas (sperm duct) and the testis artery. Collateral contribution to varicocele can be missed by surgery.
Embolisation is less invasive and there is no incisions or stitches and therefore not as painful afterward. There is no need for general anaesthetics. After embolisation you may resume normal activity in 1-2 days; after surgery, you are required to keep the wound dry and avoid strenuous activities for 1-2 weeks until the wound is healed.
Hydrocele (fluid build up around testis), infection and loss of testis are potential complications of surgery but not embolisation. Varicoceleembolisation has been performed for over 25 years; its safety and effectiveness have been shown in many studies.
It is performed by an interventional radiologist in an angiography suite as a day stay procedure. A light sedation is given. The skin is numbed by local anaesthetic. Either the jugular vein in the neck or femoral vein in the groin can be used as access. A tiny nick in the skin is made. A catheter is directed to the testicular vein under X-ray guidance. Contrast (X-ray dye) is injected to show the vein. Stainless steel or platinum coils are used to block the refluxing vein. Sclerosing foam is injected to reduce the chance of recurrence. The procedure usually takes about one hour.
You will need bed rest for 1-2 hours until the sedation is worn off. You need to arrange transport, as you are not allowed to drive for 24 hours after sedation. When you get home you should take it easy. Drink plenty of fluids. Some patients might experience back pain and scrotal pain after embolisation. This can be controlled with Panadol and Nurofen. Normal activities can be resumed the following day. Strenuous exercise should be avoided for a few days. The dressing should be kept for two days and removed afterwards. You may shower as the dressing is waterproof. We would like to see you in a month for a follow-up consultation. You should also see your urologist for further follow-up. Sperm count can be performed after three months.
Minor complications although uncommon may occur such as bruising at the entry site. Transient swelling and pain of the scrotum may occur. Loss of a coil in the lung is very rare and usually has no significant consequence. Vessel injuries are very rare.
The testes themselves are kept outside of the radiation field for testicular vein embolisation. The gonadal dose and hereditary effect is very low.